For most people, breast health and annual mammograms are almost synonymous. But what if there is more information that we should at least consider before we move forward with a traditional mammogram? There is definitely more to the story. Below we’ll cover 5 main considerations that your doctor might not mention when it comes to mammograms.
Before I begin, let me remind you that I’m not a healthcare provider, and this is not medical advice. I’m just a wife/mom who has to make decisions about healthcare screenings, and I want to have a look at the information and scientific evidence myself. I was hesitant to take on this topic because it is deeply personal to many people I know and love. Some of you have already had multiple mammograms, and some of you have already undergone cancer diagnosis and treatment. I don’t want to take anything away from your experience. Instead, my goal is to take a step back and look at the bigger picture in order to exercise discernment. I hope to do so with grace and respect for all of you, no matter your circumstances and decisions.
Consideration #1: Mammograms Give a Number of Women Cancer
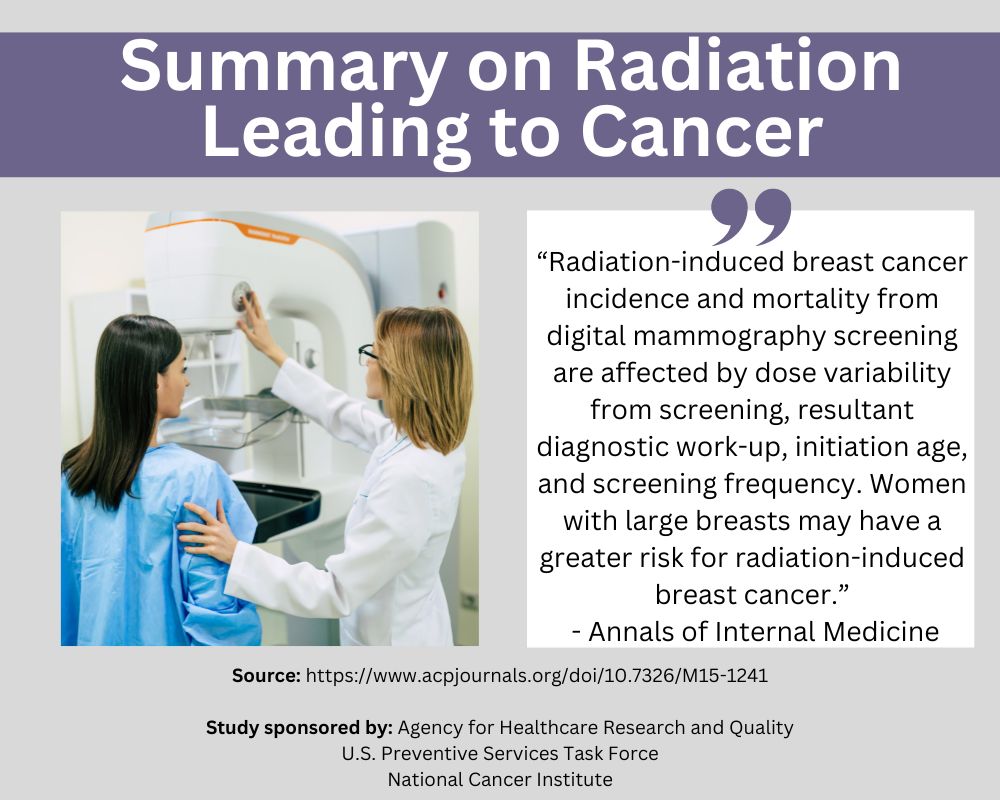
Mammogram machines emit radiation. A study published in the Annals of Internal Medicine sought to see how many cases of radiation-induced breast cancer were caused by the radiation emitted during mammogram screening process itself. While there were variations based on type of machine and breast-size of the patient, the study found that in some cases, for every 100,000 women screened, there were 266 cancer cases and 35 deaths caused by the machine’s radiation (source). That’s right. The mammogram machines themselves are giving a number of women breast cancer.
Further, the American College of Physicians explains that the accumulated lifetime exposure to radiation matters. Using modeling studies, they concluded that if a 100,000 women got a digital mammogram every year from age 40-79, the radiation exposure alone would result in 125 cases of breast cancer (source).
Simply put, the ACP has put forth a statement regarding exposure to the machine’s harmful radiation stating, “The potential harms outweigh the benefits in most women aged 40 to 49 years.” (source)
You can read much more about risk factors for radiation-induced breast cancer and radiation dose for women here. They cover radiation associated with the standard mammogram, breast density, and follow-up testing.
Consideration #2: Recommendations on Starting Age and Frequency of Mammograms Vary Greatly by Professional Organization
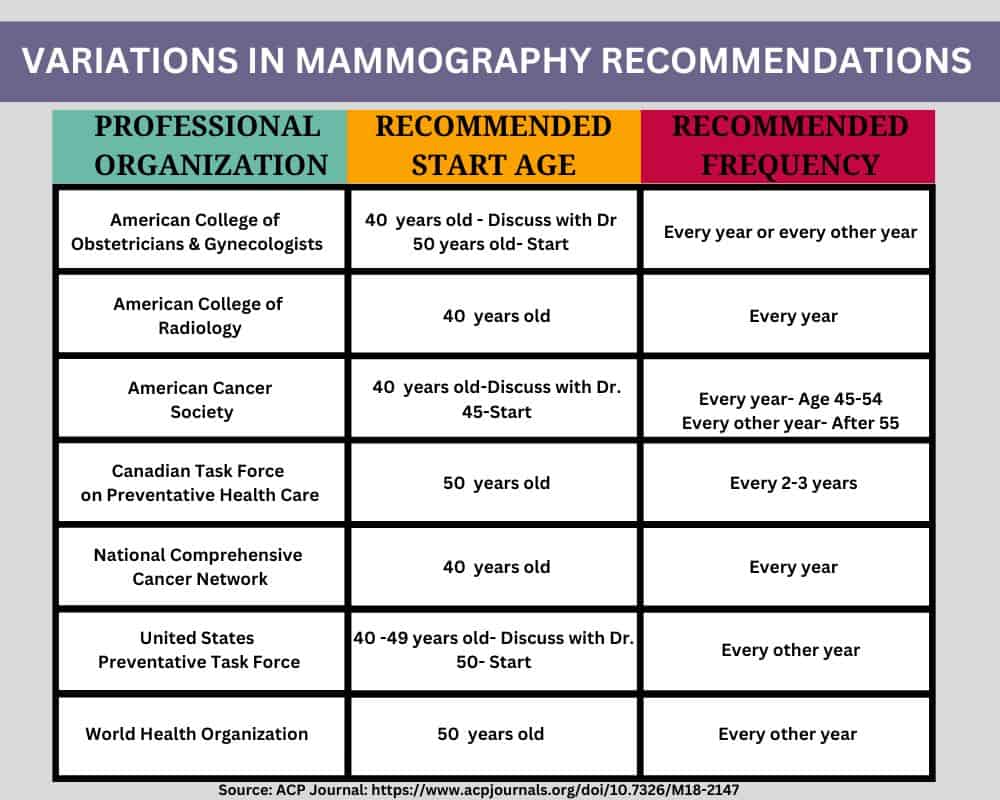
Your doctor may talk about starting age and frequency of mammograms as if a solid consensus among medical professionals has been carefully agreed upon. That just isn’t the case. Take a look at the chart below. Among the 7 different professional helath organizations, the variations in starting age for mammograms and frequency of mammograms vary significantly. Depending on if you ask the American Cancer Society or the American College of Radiology or the American College of Obstetricians & Gynecologists…you’ll get very different recommendations from each of them. The recommendations aren’t settled simply because each organization did their own risk/benefit analysis and came up with different conclusions.
Who should we listen to? The answer isn’t cut and dry. And because the answer is opinion-based, not settled science, we should at least consider the varying recommendations.
Consideration #3: There is Much Debate about Whether Mammograms Save Lives
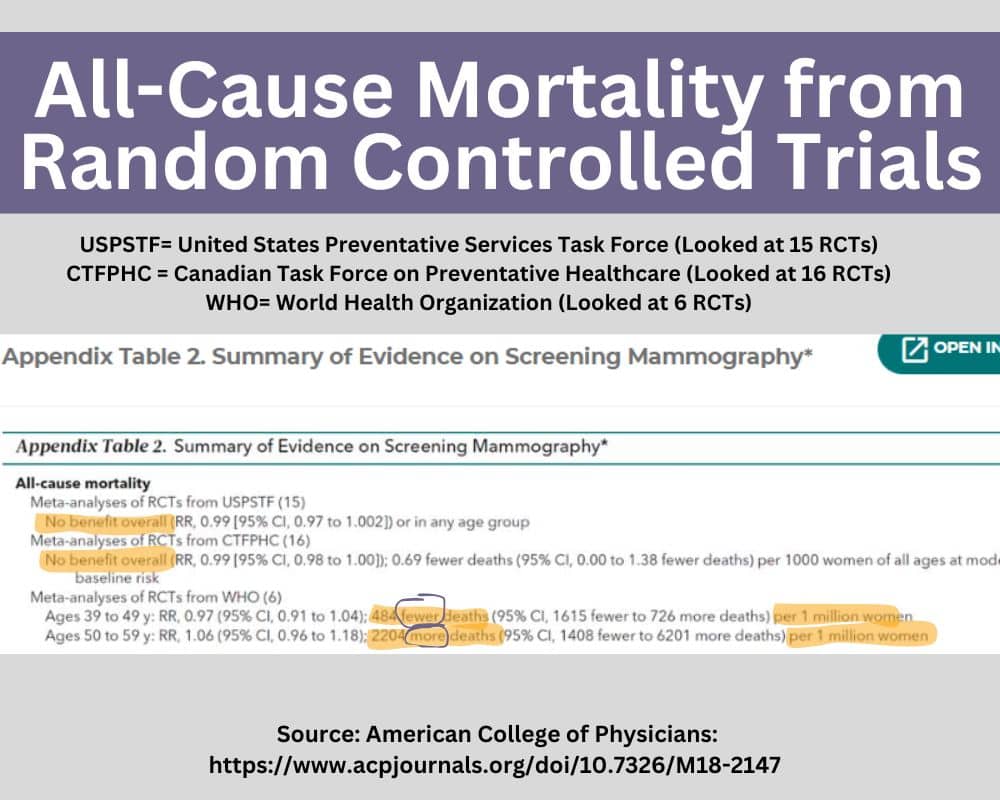
When we hear discussions that involve statistics concerning how many lives are saved through breast imaging, we first need to determine whether they are describing numbers related to breast cancer mortality OR all-cause mortality. Paying attention to all-cause mortality is much more helpful because, at the end of the day, that’s all that really matters. The trouble is most studies aren’t designed to look at all-cause mortality. They zero in on breast cancer mortality and only report that one piece of the puzzle.
The ACP sought to combine the findings from numerous studies to evaluated all-cause mortality. Their conclusion reported, “Pooled results from meta-analyses of RCTs demonstrated that mammography was not associated with a reduction in all-cause mortality” (source). The chart above shows the summary of evidence used to draw this conclusion, which was gathered from the United States Preventative Task Force (which looked at 15 Random Controlled Trails), the Canadian Task Force on Preventative Healthcare (which looked at 16 Random Controlled Trials), and the World Health Organization (which looked at 6 Random Controlled Trials).
Further, the chart below from the ACP is particularly interesting. They found that the absolute mortality reduction from breast cancer deaths thanks to mammography is about 3 deaths per 10,000 women screened over a 10 year period. At first, one might think that saving 3 lives makes it all worth it. But we can’t forget about the number of radiation-induced cancers caused by 10 years’ worth of mammograms (See Consideration #1), and the percentage of healthy women subjected to harsh, unnecessary treatments due to overdiagnosis (See Consideration #4).
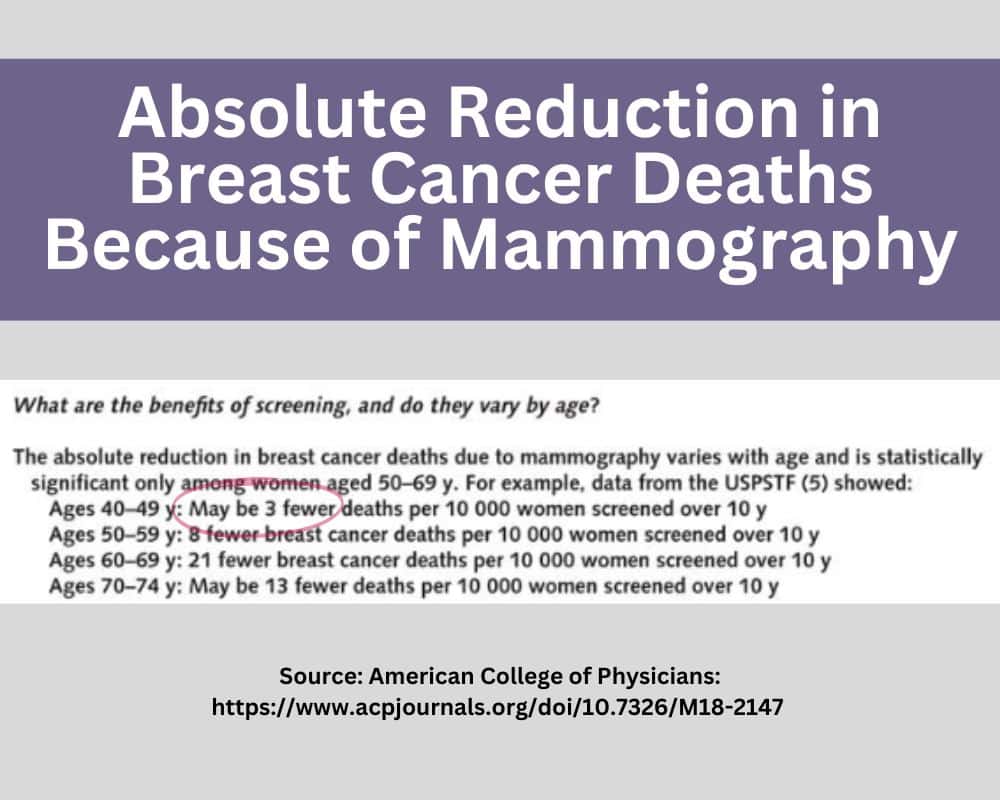
An article published in the British Medical Journal (BMJ) highlighted the conclusions from the Canadian National Breast Screening Study stating, “Annual mammography in women aged 40-59 does not reduce mortality from breast cancer beyond that of physical examination or usual care when adjuvant therapy for breast cancer is freely available.” (source)
Consideration #4: Over-Diagnosis Results in Unnecessary Treatments
There have been numerous studies that warn about over-diagnosis concerns. Over-diagnosis refers to a clinical diagnosis resulting from screening where the woman is symptom-free and would not suffer any future harm or negative health consequences if the breast is simply left alone. The Journal of Preventative Medicine published a report based on findings from the Canadian National Breast Screening Study (CNBSS). The CNBSS looked at nearly 90,000 women and reported that the over-diagnosis rate was “substantial”. They estimate that in the 40-49 age group, over-diagnosis is around 30% (source). Meaning that about 30% of the women who underwent chemo, radiation and other treatments never needed treatment to begin with.
Even worse, the NIH’s National Cancer Institute estimates that over-diagnosis could be as high as 50%. They explain, “Some screen-detected cancers are life threatening and others are not, with no definitive way of discriminating between them. Therefore, standard cancer therapies, including surgery, radiation, endocrine therapy, chemotherapy, and therapies targeting the HER2 receptor, are recommended for all cases, even for patients who will not benefit.” (source). There seems to be agreement that the highest risk for over-diagnosis is in younger women, which may be why many organizations do not advise mammography for the 40-49 years old age group.
Also, modern medicine doesn’t factor in that some tumors and lumps are handled by the body without any intervention at all. This study, published in the Archives of Internal Medicine concluded that, “Because the cumulative incidence among controls never reached that of the screened group, it appears that some breast cancers detected by repeated mammographic screening would not persist to be detectable by a single mammogram at the end of 6 years. This raises the possibility that the natural course of some screen-detected invasive breast cancers is to spontaneously regress.”
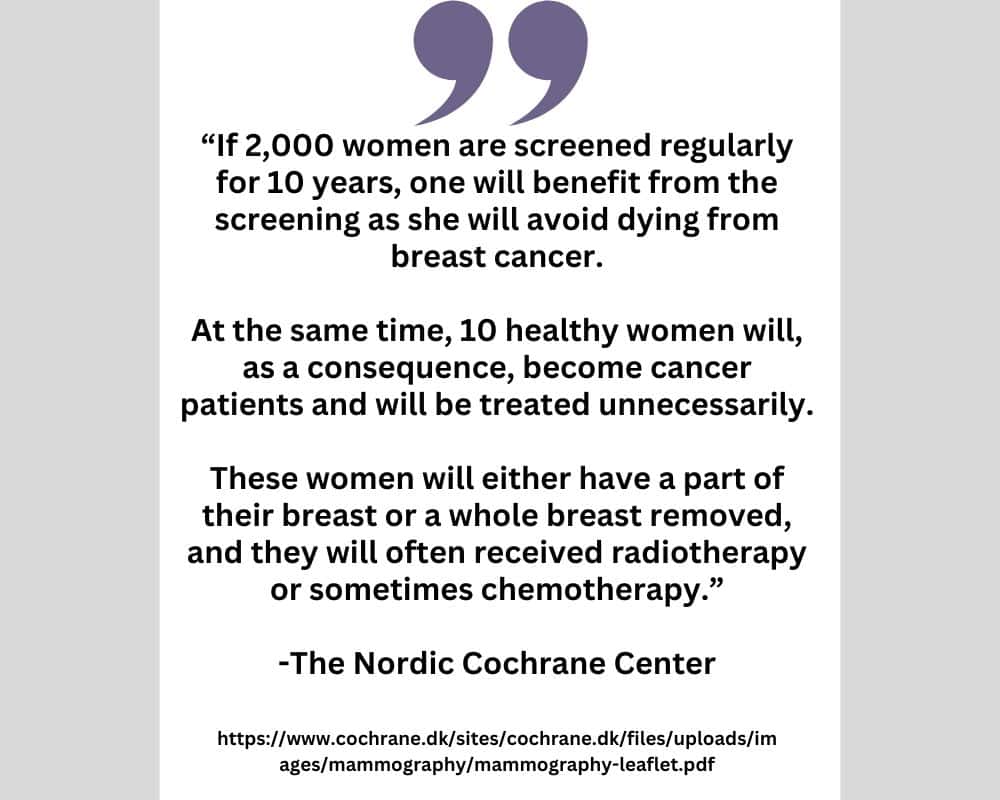
The Nordic Cochrane Center summarizes it well. They assert, ““If 2,000 women are screened regularly for 10 years, one will benefit from the screening as she will avoid dying from breast cancer. At the same time, 10 healthy women will, as a consequence, become cancer patients and will be treated unnecessarily. These women will either have a part of their breast or a whole breast removed, and they will often received radiotherapy or sometimes chemotherapy.” (source)
Consideration #5: False Positives Generate Unnecessary Fear and Expenses
While we would all agree that you can’t put a price tag on your health, we all know that each encounter with health care providers comes at a high cost. If the images of the breast indicate an issue, the women is called back in for more tests. The initial screening mammogram, the diagnostic mammogram, follow-up ultrasounds, CT scan, magnetic resonance imaging (breast MRI), biopsy… each diagnostic test your care team calls for is added to your bill. And the accumulation of those bills can quickly put a family in debt, which brings it own stress.
Many studies indicate there is a strong connection between stress-levels and many health conditions, including cancerous tumors (source). Associated stress is not limited to the family member with the diagnosis, but it could extend to the whole family.
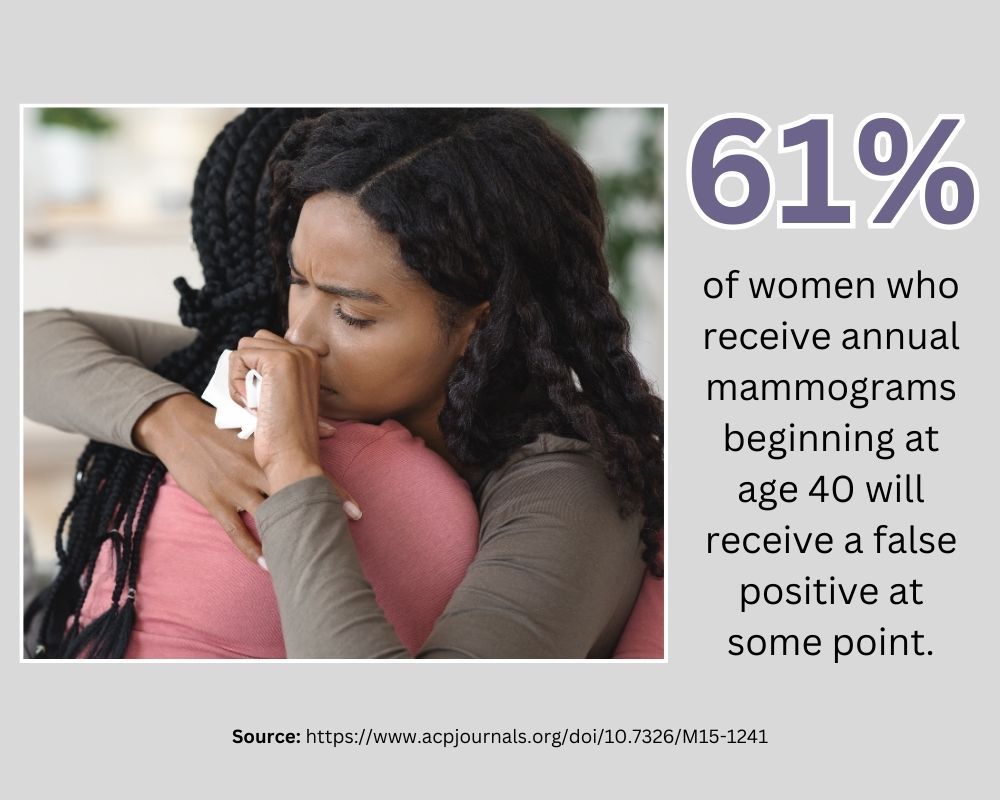
So, if one is going to take on all of that testing, expense, and stress, she would want to be sure it was warranted, right? Well, studies show that the rate of false positives with digital mammography (3 and 4 D mammograms) are significant. If a woman starts getting yearly mammograms at age 40, there is a 61% chance she’ll receive a false positive at some point! This percentage goes up to 65% for women with extremely dense breast tissue or women who use hormone therapy. (source)
Final Thoughts on Mammography

As with any medical decisions, you must do you own diligent homework. That homework should include talking to your health professionals. You should consider your own breast cancer risk based on family history of breast cancer, previous detection of cancers, genetic mutations, life expectancy, etc. But may I suggest you bring up some of these considerations presented when you have that conversation? As with any decision, it helps to fully understand both sides of the issue. And if your doctor isn’t prepared to cover some of these considerations…you can always get a second opinion!
I’ll close with a quote from the Indian Journal of Surgical Oncology, “Mammography screening programs target large numbers of healthy, asymptomatic women, and the vast majority derives no benefit from it at all. In fact, far more women are potentially harmed from mammography screening than benefit from it. It has been estimated that for every 1,000 women who undergo biennial screening mammography between the ages of 40 to 74, there will be 8 breast cancer deaths prevented, 1529 false-positive results, 213 unnecessary biopsies, and 21 over-diagnosed cases of breast cancer (4). Alternatively, for women who initiate biennial mammography screening at age 50, it is estimated that 7 breast cancer deaths will be averted, there will be 953 false-positive results, 146 unnecessary breast biopsies, and 19 over-diagnosed cases of breast cancer (source).
Now your job is to take the info, weigh the trade-offs, and make your own diligent decision!



